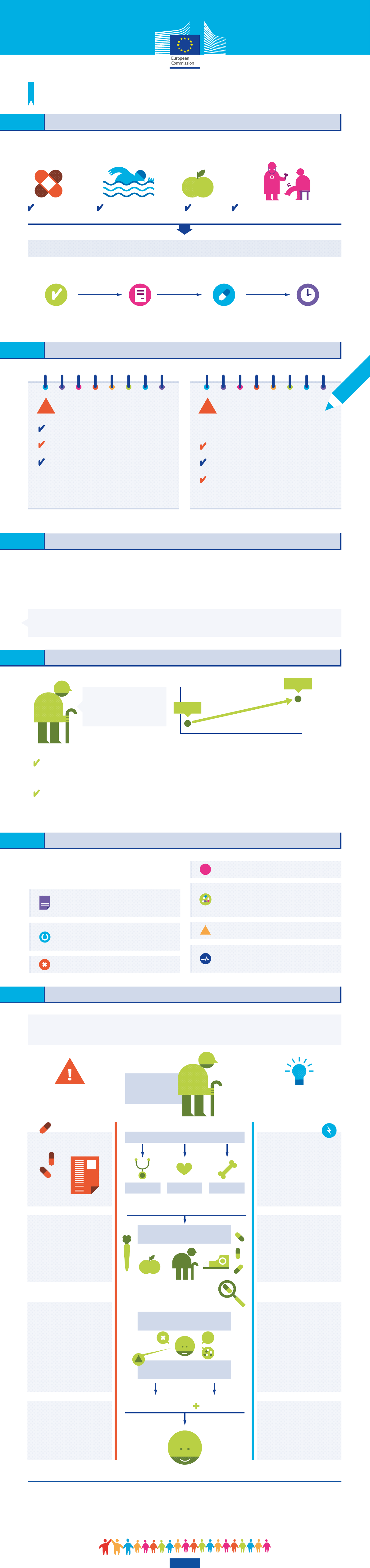
WHAT IS ADHERENCE?
Adherence to medical plans for older people
A European Innovation Partnership on Active and Healthy Ageing priority
The overall adherence process consists of:*
Adherence is the extent to which a person's behaviour corresponds with agreed recommendations
from a healthcare professional. It encompasses:
APPROPRIATENESS INITIATION IMPLEMENTATION PERSISTENCE
prescribing the right
treatment to the patient
filling the prescription
in the hospital or pharmacy
taking the medicines
following the prescription
continuing the treatment
for its whole duration
medication physical activity diet visits to health professionals
*e.g. when taking medicines
WHY ARE WE WORKING ON ADHERENCE…
… IN AN AGEING POPULATION?
of patients typically
take their medications
as prescribed
premature deaths per
year among Europeans are
related to non-adherence
"Increasing the effectiveness of adherence interventions may have a far greater impact
on the health of the population than any improvement in specific medical treatments"
Multimorbidity, the co-occurrence of multiple diseases, affects more than half
of the elderly population
Polypharmacy, the simultaneous use of multiple medicines by a single patient,
for one or more conditions, is common in older people: 40% of people aged 65
and over consume between five and nine medicines per week
Share of population
over 65 is increasing
in OECD countries:
28,4%
18,2%
28.4%
18.2%
2013 2060
Eurostat
50% 200,000
WHO report on adherence to long-term therapies
Costing statement: Medicines adherence, NICE
ONLY NEARLY
Health illiteracy (lack of understanding of one’s
condition and significance) and health beliefs
Non-adherence can be motivated
by several factors:
WHY DO PATIENTS NOT ADHERE TO THEIR MEDICAL PLANS?
Access to healthcare (e.g. cost of medication,
geographical availability)
Misunderstanding of prescription instructions
Forgetfulness
Complex regime (high number of medicines
taken at different times) or restrictive
precautions (e.g. no alcohol or cheese)
Reduction, fluctuation or disappearance
of symptoms
Adverse effects (real or imagined)
?
!
?
WHAT HAPPENS IF PATIENTS DO NOT ADHERE TO THEIR MEDICAL PLANS?
Consequences
for patients
potential harm or little clinical benefit
risks due to additional prescribing
development of resistance
to therapy (e.g. antibiotics)
!
Consequences for
the healthcare system
the cost of initial care service
medicines dispensed but not used
increased use of health services
in cases of worsening of symptoms
!
Increased health costs due to:
The European Innovation Partnership on Active and Healthy Ageing (EIP on AHA)
The European Innovation Partnership on Active and Healthy Ageing (EIP on AHA), set up in 2012, gathers stakeholders at EU, national and regional level from the public and
private sector across different policy areas. Together they share knowledge and expertise on common interests and engage in activities and projects to find innovative solutions
that meet the needs of the ageing population.
Under the framework of the EIP on AHA, the Action Group on adherence to medical plans works to improve the quality of life and health outcomes of older people by supporting
patient adherence to care plans while empowering them and delivering improvements in the healthcare system.
https://webgate.ec.europa.eu/eipaha/
• Health literacy and lifestyle
interventions (including ICT tools)
around medicines, physical activity
& nutrition
• Medication review for
appropriateness of prescription
• Web-based social platforms
• Information and counselling
campaigns
HOW ARE WE IMPROVING ADHERENCE TO MEDICAL PLANS IN OLDER PEOPLE?
hospital pharmacy
CardiologistGP Orthopaedist
Prescription of several drugs,
physical activity & nutrition advice
PROBLEMS
ENCOUNTERED
WORK UNDERTAKEN
BY THE EIP ON AHA
The European Innovation Partnership on Active and Healthy Ageing (EIP on AHA) supports public
and private actors across the EU to improve adherence to medical plans through a multidisciplinary
approach that impacts upon each step of the patient’s journey through the healthcare system.
• System works in silos
• Prescriptions not cross-checked
• Electronic prescription
• Collaborative digital platforms
between HCP
• Integrated care approaches
• Decision-support tools for
appropriateness of prescription
(e.g. guidelines, dispensing
protocols, risk stratification)
• Patient electronic health records
• Training programmes for HCP
• Patient misunderstands
the health problem or
prescription instructions
• Patient forgets to take
medication
• Patient has a complex
medication regime
• Patient misunderstands
prescription instructions
• Patient has an adverse
drug reaction
• More knowledge and evidence
needed on adherence related
issues, especially in
polymedicated patients
• Need to identify most effective
interventions
•
Electronic
devices
and alert
systems
•
Age-friendly medicines
and packaging
(e.g. Personalised
Dosage Sytems)
•
Adherence
monitoring
platforms for HCP
•
Medication review and
reconciliation protocols
•
Pharmacovigilance
tools
•
Indicators/algorithms
on
appropriate prescription, adherence
measurement, polypharmacy
•
Scientific
studies
on adherence
related issues
•
Data repositories
•
Cost-effectiveness
and
intervention analyses
Old person
with several
conditions
Focus on prescription of drugs
Patient fills in prescription of drugs
at hospital or community pharmacy
Patient seeks assistance
in case of problems with medication
?
Visits to different healthcare professionals (HCP)
?
!
H
ND-02-14-814-EN-N
 Scroll
Scroll